Drug Safety Risk Calculator
Calculate Risk Rate Like FDA Sentinel
The FDA Sentinel Initiative calculates actual risk rates by comparing observed adverse events to baseline rates. This tool demonstrates how Sentinel identifies safety concerns that traditional reporting systems might miss.
Analysis Results
Observed rate: per 1000 patients
Baseline rate: per 1000 patients
Relative risk:
Risk level:
When a new drug hits the market, doctors and patients assume it’s safe. But safety isn’t proven until millions of people use it over time. That’s where the FDA Sentinel Initiative comes in - a powerful system that uses big data to catch hidden dangers before they become public health crises.
What Is the FDA Sentinel Initiative?
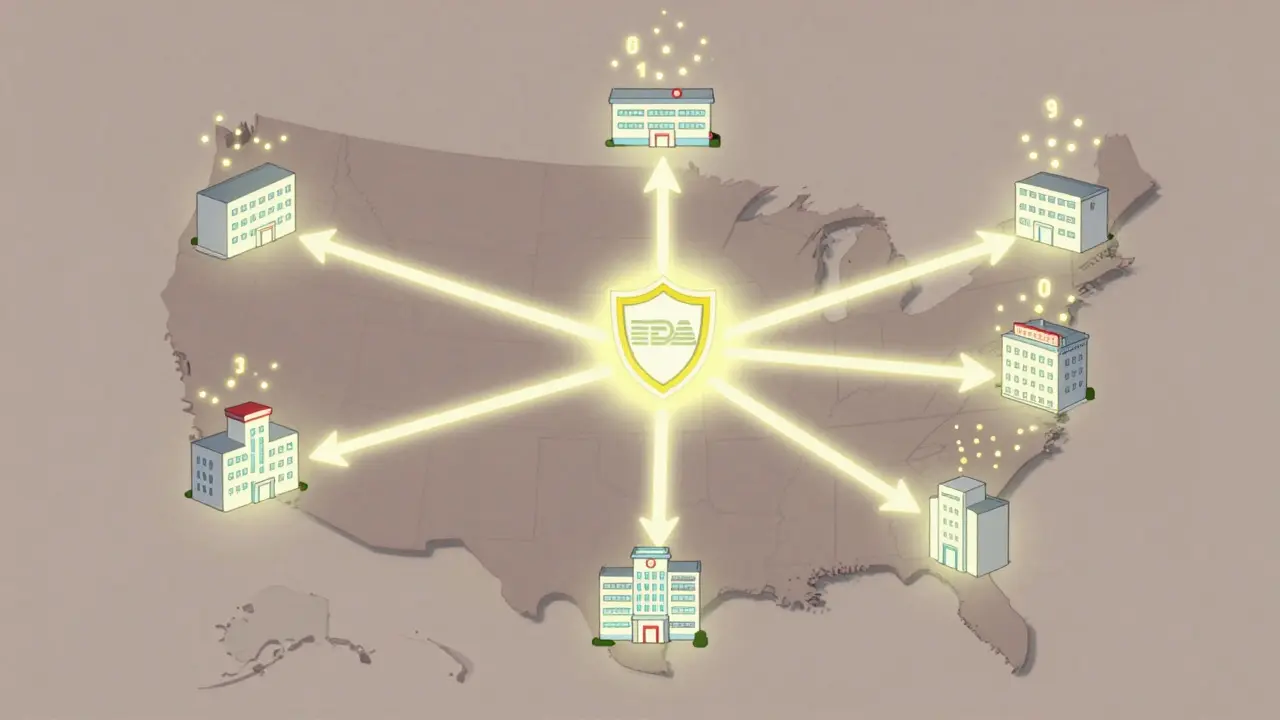
The FDA Sentinel Initiative isn’t a database you can log into. It’s a network - a distributed system that connects hundreds of healthcare organizations across the U.S. Each partner keeps its own data: insurance claims, electronic health records, pharmacy logs. The FDA doesn’t collect or store this information. Instead, it asks questions, and the system answers them where the data lives. Launched in 2008 after Congress passed the FDA Amendments Act, Sentinel was created to fix a broken system. Before Sentinel, the FDA relied on voluntary reports from doctors and patients - the FAERS database. That system got about 2 million reports a year, but most adverse events went unreported. If a drug caused a rare heart rhythm problem in elderly patients, it might take years to notice. By then, thousands could be affected. Sentinel changed that. It started as a pilot called Mini-Sentinel (2009-2015), testing whether it was possible to analyze real-world data without moving it. By 2016, the full system went live. Today, it’s the largest multisite distributed database in the world dedicated to medical product safety.How Does Big Data Find Hidden Drug Risks?
Imagine a new diabetes drug is approved. Early trials involved 5,000 people. But in the real world, 2 million people take it. Some are 80 years old. Others have kidney disease. Some take five other meds. That’s where problems hide. Sentinel looks for patterns. If, after the drug’s launch, there’s a sudden spike in hospital visits for low blood pressure among users over 70, the system flags it. It doesn’t just count cases - it compares them to what’s normal. Did 1 in 10,000 users get low blood pressure before? Now it’s 1 in 2,000? That’s a signal. The system uses data from:- Health insurance claims (billing codes for prescriptions, doctor visits, ER trips)
- Electronic health records (EHRs) - including doctor’s notes, lab results, diagnoses
- Pharmacy records (what meds patients actually picked up)
Why Is This Better Than Old-School Reporting?
Traditional systems like FAERS are like listening for whispers in a storm. People don’t report side effects unless they’re severe, obvious, or they know how to file a report. Many don’t connect their symptoms to a drug. Others assume it’s just aging. Sentinel doesn’t wait for whispers. It listens to the whole room. Here’s how it beats the old way:- Denominator data: Sentinel knows how many people took the drug. FAERS doesn’t. If 10 people had a reaction out of 100,000 users, that’s 0.01%. But if 10 people had it out of 1,000? That’s 1% - a red flag.
- Speed: Traditional studies take years. Sentinel can detect a signal in weeks.
- Real populations: Clinical trials exclude the elderly, pregnant women, and people with multiple conditions. Sentinel includes them.
- Scale: It covers over 200 million people across the U.S. - more than half the population.

How Does the System Stay Secure and Private?
Data never leaves its source. That’s the core principle. A hospital in Chicago, an insurance company in Texas, a clinic in Florida - they all keep their own data. The FDA sends a query: “Show me all patients over 65 who took Drug X and had a stroke in the last 90 days.” Each partner runs the same program on their own servers. They return only the results - no names, no addresses, no Social Security numbers. Just numbers: “127 patients had strokes.” This distributed model protects privacy and avoids legal hurdles. It also makes the system harder to hack. There’s no central server full of sensitive records to break into. But it’s not perfect. Different systems use different codes for the same condition. One hospital calls it “heart failure,” another says “congestive cardiac failure.” Sentinel’s Innovation Center spends millions fixing these mismatches - a process called feature engineering.What’s Next? AI, EHRs, and Global Expansion
In 2019, the FDA split Sentinel into three teams:- Sentinel Operations Center: Runs the daily queries and safety checks.
- Innovation Center: Builds the next-gen tools - using AI to read doctor’s notes, spot patterns in unstructured text.
- Community Building Center: Trains researchers and helps partners join the network.
- AI for clinical notes: Doctors write “Pt. feels dizzy after starting med.” AI is learning to turn that into structured data - “dizziness, onset within 48 hours of drug initiation.”
- Real-world trial emulation: Can Sentinel mimic a clinical trial using real data? Yes. In 2021, it replicated a major diabetes drug trial with 97% accuracy.
- Causal inference: Not just correlation. Can it prove Drug X caused the reaction? New statistical models are getting closer.

Who Uses Sentinel - And Why It Matters
It’s not just the FDA. Pharmaceutical companies use it to monitor their own drugs. Academic researchers run studies through it. The CDC uses it for vaccine safety. Even international agencies like the EMA (European Medicines Agency) are studying Sentinel’s model to build their own systems. That’s the real power: it’s not just a tool. It’s infrastructure. Like the highway system or the power grid, it’s something society runs on - quietly, behind the scenes. For patients, it means safer drugs. For doctors, it means better guidance. For regulators, it means acting before the next crisis.Limitations - What Sentinel Can’t Do
Sentinel isn’t magic. It has limits:- Rare events: If a side effect happens in 1 in 500,000 people, even Sentinel might miss it. You still need large, long-term studies.
- Data gaps: If someone gets a reaction at home and never sees a doctor, it won’t show up.
- Complex interactions: If five drugs interact in a weird way, it’s hard to isolate the culprit.
- Learning curve: Researchers need training to use the system properly. It’s not a Google search.
Why This Matters to You
You might never hear about Sentinel. But if you or a loved one takes a prescription, gets a vaccine, or uses a medical device - it’s watching. It’s the reason some drugs get stronger warnings. The reason some are pulled off the market. The reason new ones are safer than ever. It turns passive reporting into active protection. It turns scattered data into life-saving insight. And it does it all without ever seeing your name. The FDA Sentinel Initiative isn’t just technology. It’s trust - built on data, protected by design, and powered by the quiet work of thousands of health systems across America.How does the FDA Sentinel Initiative differ from FAERS?
FAERS relies on voluntary reports from doctors and patients, which leads to underreporting and lacks data on how many people used a drug. Sentinel uses real-world data from millions of patients across healthcare systems, allowing it to calculate actual risk rates and detect patterns automatically - without waiting for someone to report an issue.
Does Sentinel collect personal health information?
No. Sentinel never collects or stores personal data. Each participating organization keeps its own records. The FDA sends analytical queries, and the results - stripped of identifiers - are returned. Only aggregated numbers are shared, never names, addresses, or Social Security numbers.
Can Sentinel detect side effects in elderly or pregnant patients?
Yes. Clinical trials often exclude these groups, but Sentinel includes them because it uses real-world data. This means it can spot risks in older adults, pregnant women, and people with multiple health conditions - populations that traditional studies miss.
How long does it take for Sentinel to find a drug safety issue?
Traditional studies can take years. Sentinel can detect a potential safety signal in weeks. For example, a spike in hospital visits linked to a new drug might be flagged within 30 days of launch, allowing the FDA to act much faster than before.
Is Sentinel used outside the U.S.?
Not directly, but it’s being studied as a model. Agencies like the European Medicines Agency and Health Canada are building similar distributed systems based on Sentinel’s architecture. Its success has made it the global benchmark for post-market drug safety monitoring.

Write a comment