When your kidneys aren’t working right, it’s not just about urinating less or feeling tired. The real danger comes from what builds up in your blood-too much phosphorus, too much fluid, or blood clots that can cause a stroke or heart attack. That’s where phosphate binders, diuretics, and anticoagulants come in. These aren’t optional extras. They’re the backbone of keeping people with advanced kidney disease alive and out of the hospital.
Phosphate Binders: Stopping Phosphorus Before It Hits Your Blood
Your kidneys normally filter out phosphorus from the food you eat. When they fail, phosphorus piles up. Over 60% of people with stage 4 or 5 chronic kidney disease (CKD) have high phosphorus levels, according to the National Kidney Foundation. That doesn’t just cause itchy skin or bone pain. Too much phosphorus hardens your arteries, speeds up heart disease, and doubles your risk of dying.
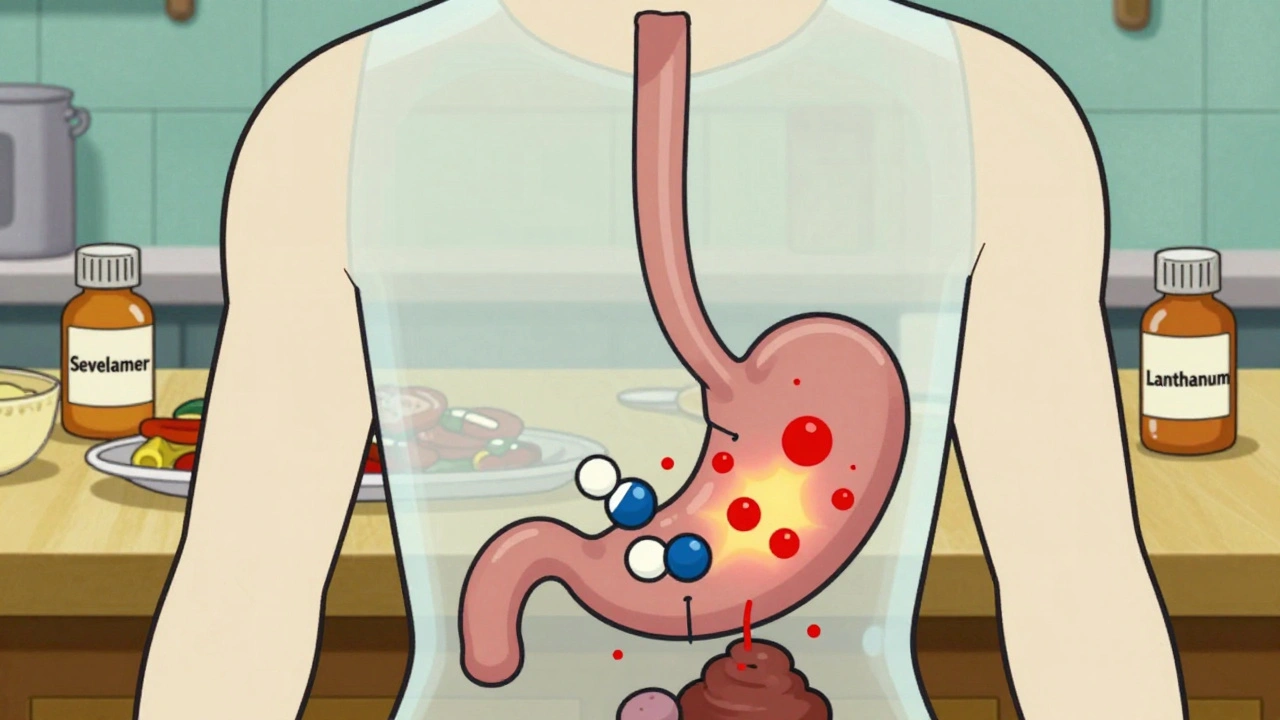
Phosphate binders don’t fix your kidneys. They work in your gut. They grab onto phosphorus from your food and carry it out in your poop instead of letting it absorb into your blood. You take them with every meal and snack-no exceptions.
There are four main types:
- Calcium-based (calcium acetate, calcium carbonate): Cheap, around $50-$80 a month in the U.S. But they can raise your calcium levels, leading to dangerous calcification in your heart and blood vessels.
- Sevelamer (Renagel, Renvela): Doesn’t affect calcium. Studies show it lowers death rates by 18% in dialysis patients. But it costs $120-$200 AUD monthly without subsidies and often causes severe constipation.
- Lanthanum carbonate (Fosrenol): Also calcium-free. Fewer GI side effects than sevelamer. Costs about the same.
- Iron-based (ferric citrate, sucroferric oxyhydroxide): A two-for-one deal. Lowers phosphorus and boosts iron levels. Ferric citrate (Auryxia) costs $6,500-$7,200 a year. Newer, but expensive.
The KDIGO 2023 guidelines say: avoid calcium binders if your calcium is already high. Start with sevelamer or lanthanum. But cost and side effects make adherence terrible-42% of patients quit within six months. One Reddit user switched from sevelamer to lanthanum after constipation landed them in the ER. It worked better, but the out-of-pocket cost was brutal.
Diuretics: Fighting Fluid Overload and High Blood Pressure
Eighty to ninety percent of people with CKD have fluid overload. That means swollen ankles, shortness of breath, and blood pressure that won’t budge-even with three different pills. Diuretics flush out the extra fluid through your urine.
Loop diuretics are the first line: furosemide, bumetanide, torsemide. They work even when kidney function is low, down to an eGFR of 15. Thiazides like metolazone help too, but only if your eGFR is above 30.
Here’s the catch: many patients develop diuretic resistance. Your body gets used to it. That’s why doctors often combine torsemide with metolazone. Torsemide is 30% more bioavailable than furosemide, meaning a 20mg dose equals 40mg of furosemide. It lasts longer, too-so fewer bathroom trips at night.
But here’s what patients actually deal with:
- Furosemide: $4-$10 a month generic. First choice because it’s cheap.
- Torsemide: $10-$25 generic, $90-$120 brand. Preferred by 62% of patients in a 2022 survey for fewer nighttime trips.
- Metolazone: Added when loop diuretics stop working. Dose: 2.5-5mg daily.
The FIRST trial showed torsemide cut heart failure hospitalizations by 22% compared to furosemide. But most doctors still start with furosemide because it’s been around since the 1960s and everyone knows how to use it.
Patients say the biggest problem isn’t the pill-it’s the timing. Taking diuretics after 4 p.m. means waking up three times a night to pee. Splitting the dose-half in the morning, half at lunch-helps. Sixty-five percent of experienced users swear by it.

Anticoagulants: Preventing Clots When Your Kidneys Are Failing
People with CKD have a 2-4 times higher risk of stroke and heart attack than the general population. Why? Their blood clots more easily. That’s where anticoagulants come in.
Two main groups: warfarin (old-school) and DOACs (newer: apixaban, dabigatran, rivaroxaban, edoxaban).
Warfarin needs weekly blood tests (INR checks). But here’s the surprise: in advanced CKD (eGFR under 15), warfarin is often more predictable than DOACs. That’s because DOACs rely on the kidneys to clear them, and when kidneys are this bad, levels can spike unpredictably.
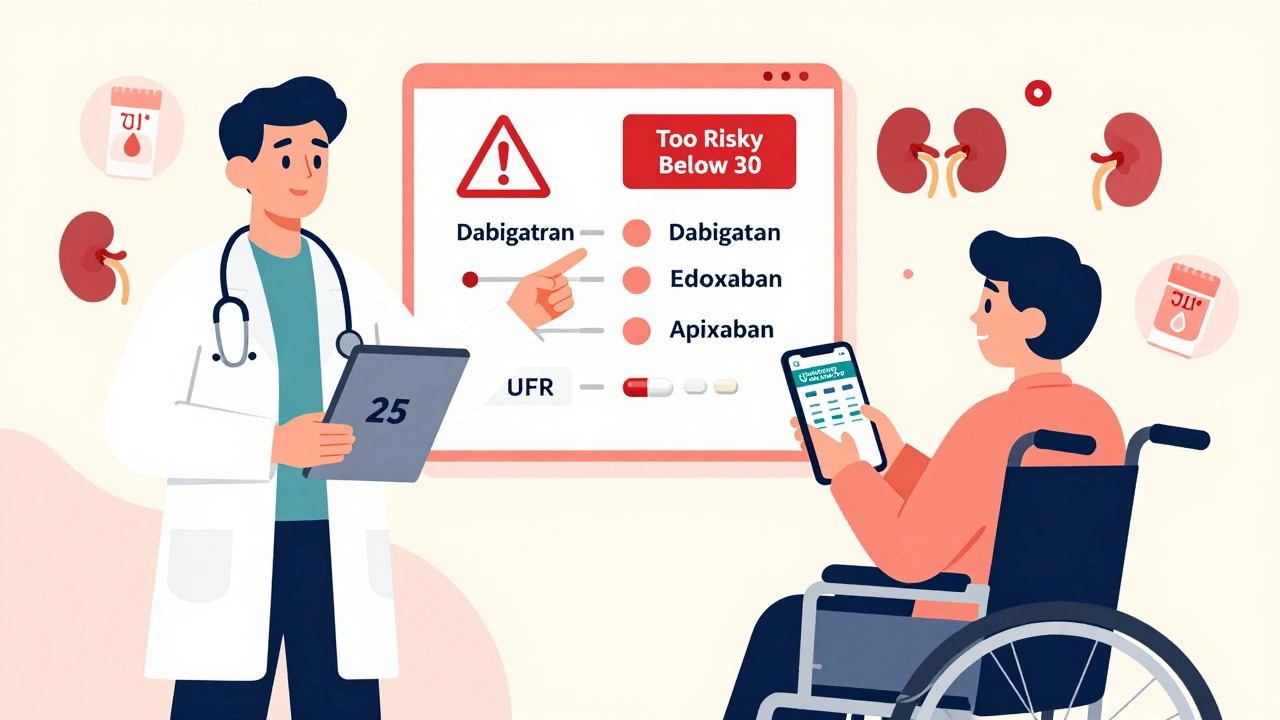
DOACs are preferred if your eGFR is above 30. But dosing changes with kidney function:
- Apixaban (Eliquis): Standard dose is 5mg twice daily. For eGFR 15-29, cut to 2.5mg twice daily. It’s the only DOAC approved for eGFR as low as 15. The ARISTOTLE trial showed 31% less major bleeding than warfarin.
- Dabigatran (Pradaxa): Not recommended below eGFR 30. Higher bleeding risk in moderate CKD.
- Rivaroxaban (Xarelto): Dose drops to 15mg daily if eGFR is 15-50.
- Edoxaban (Savaysa): Contraindicated below eGFR 15.
Apixaban is now the go-to for most CKD patients with atrial fibrillation and eGFR above 25. It’s safer than warfarin and doesn’t need constant blood tests. But bleeding is still a real concern. One user on HealthUnlocked switched from apixaban to warfarin after alarming bruising. “Warfarin meant weekly blood draws,” they said, “but I knew exactly where I stood.”
Only 35% of primary care doctors dose anticoagulants correctly in CKD, according to JAMA Internal Medicine. That’s why tools like the National Kidney Foundation’s “Medicines and CKD” app-downloaded 150,000 times-are so valuable. It reduces medication errors by 27%.
What Works Best? The Real-World Trade-Offs
There’s no perfect choice. It’s about balancing safety, cost, and lifestyle.
Phosphate binders: If you’re young and can afford it, sevelamer or lanthanum reduce long-term death risk. If you’re on a tight budget and your calcium is low, calcium acetate is fine-but monitor levels closely.
Diuretics: Start with generic furosemide. If you’re still swollen or your BP won’t drop, add metolazone or switch to torsemide. Split your dose to avoid sleepless nights.
Anticoagulants: If your eGFR is above 30, apixaban is your best bet. If it’s below 15, warfarin is still the most studied and reliable. Never assume a DOAC is safe just because it’s newer.
And here’s the hard truth: even the best meds won’t help if you don’t take them right. A 2022 study found 70% of people stop phosphate binders within six months-not because they didn’t work, but because they forgot, hated the side effects, or couldn’t afford them.
What’s Changing in 2025?
The landscape is shifting fast. In September 2023, the FDA approved tenapanor (Xphozah), a new kind of phosphate binder that works differently-blocking phosphate absorption in the gut instead of binding it. Early data shows it reduces phosphorus 30% more than sevelamer. But it costs $6,800 a year.
SGLT2 inhibitors like dapagliflozin (Farxiga) and empagliflozin (Jardiance) are now first-line for CKD patients with diabetes. They reduce phosphate levels naturally, which means fewer phosphate binders needed. In trials, they cut phosphate binder use by 15-20%.
On the anticoagulant front, the AUGUSTUS-CKD trial showed that using apixaban with just one blood thinner (not two) cuts bleeding risk by 31%. That’s huge for people already on multiple meds.
And a new diuretic, AZD9977, is in phase 3 trials. If it works, it could solve the biggest problem in advanced CKD: diuretic resistance.
But the big question remains: can we afford this? The average annual cost of optimal CKD meds-binders, diuretics, anticoagulants, SGLT2 inhibitors-can hit $10,000 or more. That’s unsustainable for most healthcare systems. Yet, the American Society of Nephrology estimates that following current guidelines could save $12 billion a year by delaying dialysis and preventing heart attacks.
What Should You Do?
If you or someone you care for has advanced kidney disease:
- Get your serum phosphorus, calcium, and eGFR checked every 3 months.
- Take phosphate binders with every bite of food-not before, not after.
- Ask your doctor if torsemide or a diuretic combo might work better than furosemide alone.
- For anticoagulants, confirm your eGFR and ask: is apixaban the right choice? Or should we stick with warfarin?
- Use the NKF’s “Medicines and CKD” app to check doses. It’s free and trusted by nephrologists.
- Don’t stop meds because they’re expensive or inconvenient. Talk to your doctor. There are patient assistance programs. There are generics. There are alternatives.
Kidney disease doesn’t have a cure. But with the right meds, taken right, you can live longer, feel better, and avoid the ER. That’s not magic. That’s medicine.

Write a comment