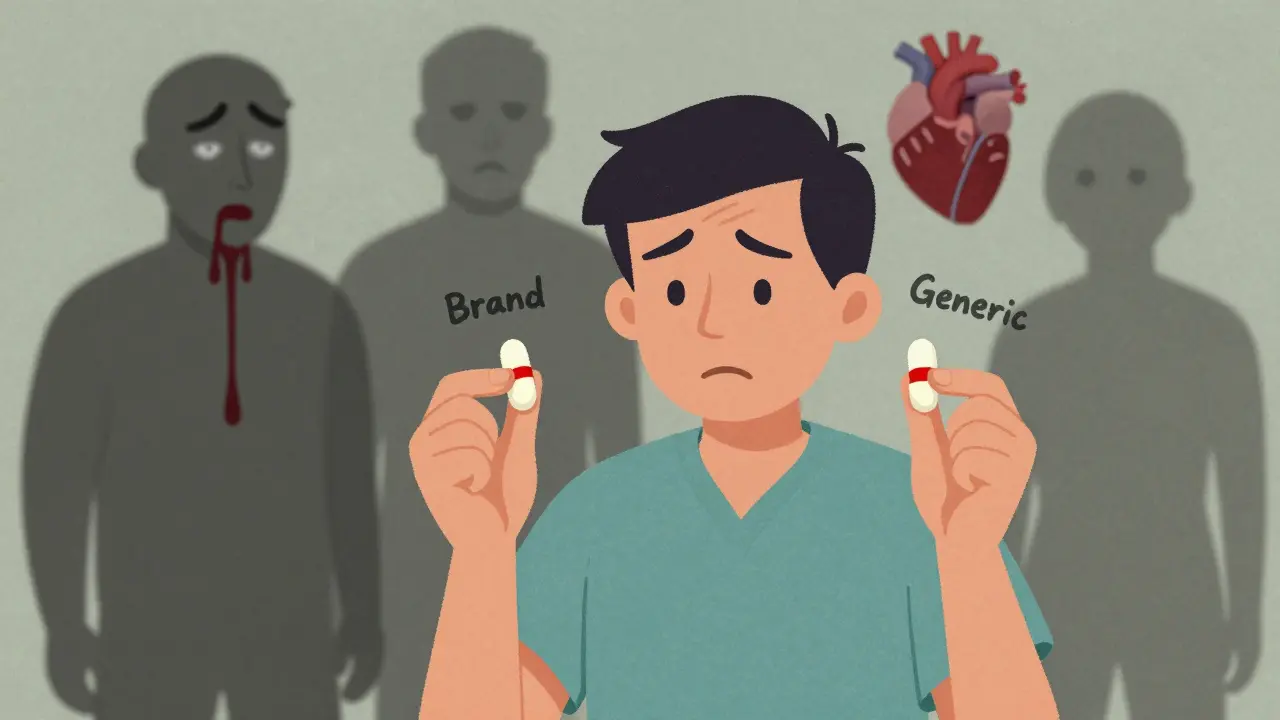
It’s supposed to be the same drug. Same active ingredient. Same price. So why does it sometimes feel like your generic medication just… doesn’t work?
For millions of people taking generics for conditions like epilepsy, heart disease, or cancer, the expectation is simple: a generic should act just like the brand-name version. But in real life, that’s not always true. And when it fails, the consequences aren’t just inconvenient-they can be deadly.
What Exactly Is a Therapeutic Failure?
A therapeutic failure happens when a drug doesn’t do what it’s supposed to. Your blood pressure stays high. Your seizures return. Your cancer keeps growing. You’re taking the right medicine, on schedule, but your body isn’t responding. And if you’ve recently switched from a brand-name drug to a generic, that switch might be the cause.
The FDA says generics are bioequivalent to brand-name drugs. That means they must deliver the same active ingredient at a similar rate and amount. But here’s the catch: the acceptable range for that similarity is 80% to 125%. In plain terms, a generic could deliver up to 20% less-or 25% more-of the active ingredient than the original. For most drugs, that’s fine. For others, it’s a gamble.
The Dangerous Edge: Narrow Therapeutic Index Drugs
Some medications have a razor-thin line between helping you and harming you. These are called Narrow Therapeutic Index (NTI) drugs. Examples include warfarin (a blood thinner), phenytoin (for seizures), digoxin (for heart rhythm), and tacrolimus (for transplant patients).
With these drugs, a 10% difference in dose can mean the difference between life and death. Too little? A clot forms, or your body rejects the new organ. Too much? You bleed internally or suffer toxic organ damage.
That’s why experts argue the standard 80-125% bioequivalence range is too loose for NTI drugs. The FDA has started requiring tighter standards-90% to 111%-for some of these, but not all. And even then, manufacturing flaws can still slip through.
In 2024, researchers found that multiple sclerosis patients who relapsed had been taking generics containing as little as 72.5% of the labeled dose. Those who stayed stable? Their generics contained 97% to 103%. That’s not random variation. That’s inconsistent quality.
Why Do Generics Fail? It’s Not Just the Active Ingredient
People assume the only thing that matters is the active pharmaceutical ingredient (API). But that’s not the whole story. The fillers, binders, coatings, and dissolution rates matter just as much.
Take Budeprion XL, a generic version of Wellbutrin. In 2013, the FDA pulled it off the market after hundreds of patients reported severe side effects-headaches, anxiety, even suicidal thoughts. The problem? The inactive ingredients changed how the drug released into the body. Instead of a steady 12-hour release, it dumped the full dose all at once. The API was correct. The delivery system wasn’t.
Same thing happened with generic Concerta for ADHD. Some versions dissolved too fast. Others didn’t dissolve enough. Patients went from focused to lethargic-or worse, jittery and agitated.
Manufacturing flaws are common. About 31% of deficiencies in generic drug applications come from production issues. That includes uneven mixing of ingredients, poor tablet compression, or unstable coatings that break down too soon in the stomach.
And it’s not just one batch. Investigators found pills from the same blister pack contained wildly different amounts of active drug-some 30% under, others over the label amount. That’s not a one-off mistake. That’s systemic.

The Silent Threat: Degradation and Contamination
Drugs don’t stay perfect forever. They degrade. Heat, humidity, light-they all eat away at the active ingredient over time.
Hydrolysis (breakdown by moisture) is common in ester-based drugs. Oxidation ruins others. Photolysis? That’s when light breaks the molecule apart. If a generic isn’t stored right-or if the packaging doesn’t protect it-your pill might be half-dead by the time you take it.
Then there’s contamination. In recent years, the FDA has recalled dozens of blood pressure meds-valsartan, losartan, irbesartan-because they contained cancer-causing nitrosamines. Ranitidine (Zantac) was pulled for the same reason. These weren’t manufacturing errors. They were chemical byproducts that slipped through testing.
One former FDA officer put it bluntly: “Valsartan is just the one we caught. Who knows how many more are out there?”
Who’s Affected? Real Stories, Real Risks
Doctors in the U.S., Canada, and Europe have reported patients whose cancer treatment stopped working after switching to a generic chemo drug. One patient described her tumor growing back within weeks. Another had to stop treatment entirely because the generic caused unbearable nausea and nerve damage.
In May 2024, Glenmark Pharmaceuticals recalled nearly 47 million potassium chloride tablets. Why? They weren’t dissolving properly. Patients with low potassium-already at risk for heart arrhythmias-were getting nothing. Some were hospitalized.
One heart transplant patient, Salberg, noticed her symptoms returning after switching to a generic immunosuppressant. She wondered: “If the drug dumped into my system too quickly, did it wear off too soon?” That’s the nightmare scenario-your body rejects the new organ because the drug didn’t last.
And it’s not just the patients. Pharmacists are seeing it too. A pharmacist in Ohio described a patient who overdosed on methotrexate after switching generics. The new version released the drug faster. The patient ended up in the ER.

The Supply Chain Problem
Most generic drugs aren’t made in the U.S. Over 80% of the active ingredients come from India and China. Regulatory oversight there is uneven. Some factories meet U.S. standards. Others don’t.
The FDA inspects only a fraction of overseas facilities each year. And when they find problems, the response is often slow. A drug might be recalled months after patients have already taken bad batches.
Then there are the middlemen-Pharmacy Benefit Managers (PBMs). They negotiate drug prices with manufacturers and pharmacies. But their contracts often push pharmacists to dispense the cheapest generic, even if it’s not the most reliable. Patients pay less at the counter-but pay more in health risks.
As one expert put it: “The same lack of transparency causing outrage over branded drug prices is also creating issues in the generic market.”
What Should You Do?
If you’re on a generic drug and you feel something’s off-your symptoms are returning, you’re having new side effects, or you’re just not feeling right-talk to your doctor. Don’t assume it’s your condition worsening.
Ask: “Could this be the generic?”
Keep a symptom journal. Note when you switched medications. Track changes in energy, mood, pain, or function. Bring it to your appointment.
If you’re on an NTI drug-warfarin, digoxin, levothyroxine, phenytoin-ask if your pharmacy can stick with the same brand or generic manufacturer. Some pharmacies let you request a specific maker. It’s worth asking.
Don’t be afraid to go back to the brand-name version if needed. Insurance may push back, but your health comes first. Many insurers will cover the brand if you document therapeutic failure.
And if you’re prescribed a new generic, check the pill’s appearance. Compare it to your old one. If the shape, color, or imprint changed, ask why. That’s not just cosmetic-it might mean a different manufacturer, different formulation, different risk.
The Bigger Picture
Generics saved the U.S. healthcare system billions. They’re essential. But they’re not all created equal. The system assumes that bioequivalence = clinical equivalence. But biology doesn’t always follow the math.
Until regulatory standards tighten for high-risk drugs, and until supply chains become transparent, patients will keep paying the price for cost-cutting.
There’s no perfect solution. But awareness is the first step. If you’re taking a generic and something feels wrong-trust yourself. Your body knows.

Write a comment